Where Does Legionnaires’ Disease Come From?
Understanding How Legionella Bacteria Spreads and Causes Outbreaks

One of the first questions victims ask is, “How did I get Legionnaires’ disease?” Legionnaires’ disease comes from inhaling Legionella bacteria that originate in water or soil. Unlike many illnesses, it’s not passed person-to-person – the source is environmental, typically a man-made water system. Identifying where the Legionella came from is critically important, both for stopping an outbreak and for holding the right people accountable in a Legionnaires’ disease lawsuit.
Legionella bacteria thrive in warm, stagnant water with poor or no disinfectant. When that water turns into tiny droplets (mist or vapor), people can breathe it in and get sick. Any building or device that stores and disperses water can become the breeding ground for Legionella if not properly maintained. Below are the most common sources of Legionnaires’ disease outbreaks:
On Vacation: Hotels, Resorts, Vacation Rentals (AirBNB, VRBO) and Cruise Ships
Places we stay during travel – hotels, motels, resorts, and cruise ships – are frequent sites of Legionnaires’ disease outbreaks. These venues often have complex water systems and amenities that can harbor Legionella, such as hot tubs, spas, swimming pools, decorative fountains, and large HVAC cooling towers for air conditioning.
- Hot tubs & spas: A hot tub’s warm water is an ideal environment for Legionella. If the tub isn’t cleaned and chlorinated enough, bacteria can grow. The bubbling water creates a mist that can carry Legionella into the air. There have been outbreaks where hotel whirlpool spas were identified as the source – dozens of guests inhaled contaminated steam and became ill.
- Cooling towers & AC systems: Many large hotels use cooling towers (part of the air-conditioning system) to regulate temperature. These towers contain warm water basins. If not regularly disinfected, Legionella can grow there and then spread through the building’s ventilation. For example, the very first recorded Legionnaires’ outbreak in 1976 was traced to a hotel’s cooling tower on its air conditioning system (Where Does Legionnaires’ Disease Come From? – Legionnaires’ Disease Attorney) (Where Does Legionnaires’ Disease Come From? – Legionnaires’ Disease Attorney). That outbreak sickened over 200 people and caused 34 deaths at a Philadelphia hotel hosting an American Legion convention – which is how the disease got its name.
- Low occupancy issues: Hotels or cruise ships that have low occupancy or are temporarily closed (for instance, offseason or during pandemics) face a risk: water sits unused in pipes and tanks for long periods. Stagnant water + warm temperatures = Legionella growth. In fact, when buildings reopened after COVID-19 lockdowns, health officials saw a spike in Legionnaires’ disease cases linked to water that sat in hotels and gyms (Where Does Legionnaires’ Disease Come From? – Legionnaires’ Disease Attorney). Tip: If you’re checking into a hotel room that’s been unoccupied, running the shower and taps hot for several minutes (and leaving the room during that time) can help flush the system – a good precaution, though ultimately it’s the hotel’s responsibility to maintain safe water.
Who is responsible? Hotels and cruise lines are expected to have water maintenance plans. If you caught Legionnaires’ at a hotel or on a cruise, the property owner or operator could be liable for negligence. Our legal team has successfully sued resort hotels for Legionnaires’ disease – including obtaining a $6.45 million recovery for victims of a recent Legionnaires” outbreak at a hotel.
Hot Tubs, Pools, and Water Play Areas
Any recreational water that isn’t adequately disinfected can become a Legionella breeding ground. This category overlaps with some of the above settings but focuses on the equipment itself:
- Public Hot Tubs & Spas: Beyond hotels, think of gyms, community centers, cruise ships, or rental vacation homes with hot tubs. If you used a hot tub and developed pneumonia afterward, Legionella from the tub could be the cause. Public hot tubs are required to be maintained to health codes, but not all are. The warm (around 37°C / 98°F) temperature and aeration make them prime Legionella incubators. Always check if the facility logs daily chlorine/bromine checks; if you don’t see proof of maintenance, be cautious.
- Swimming Pools: While less common (pools are usually cooler and more chlorinated), indoor pools or therapy pools (which may be warmer) can harbor Legionella, especially in the filters or heating systems. Also, if a pool has a waterfall feature or spa attachment, those areas could aerosolize water.
- Water Parks & Fountains: Splash pads or water playgrounds, decorative fountains, misters (like those in theme parks or on city streets in summer) – these have caused outbreaks too. Kids can get Legionnaires’ disease from inhaling mist at a splash park if the water isn’t properly treated (there was a notable case of this in Kansas a few years back). Even though Legionnaires’ is more common in older adults, children and young people can contract it if the exposure is high.
For all these, the common thread is negligence in maintenance. Owners must keep equipment clean and water properly sanitized. When they don’t, legal action may be the only way to hold them accountable and prompt safer practices.
Hospitals, Nursing Homes and Long-Term Care Facilities
It’s especially tragic when the place people go to get healthier ends up making them sick. Unfortunately, hospitals, nursing homes and long-term care facilities are common sources of Legionnaires’ disease outbreaks. In fact, a CDC review found that healthcare-associated Legionnaires’ disease (cases caught in hospitals or nursing homes) made up 25% of all Legionnaires’ cases and were more likely to be deadly.
Why are hospitals and care facilities at risk?
- They often have large, complex plumbing systems – with many rooms, wings, and floors. If any part of that water system isn’t hot enough or chlorinated enough, Legionella can grow. Parts of the system like hot water tanks, decorative fountains in lobbies, physical therapy pools, or even medical equipment (like respiratory devices that use water) can harbor bacteria. There have been cases where a nursing home’s rehab whirlpool tub was the culprit, or the facility’s water heaters were kept at too low a temperature to save on energy costs (unintentionally creating ideal Legionella conditions).
- Patients in hospitals and seniors in nursing homes are usually more vulnerable due to age or underlying health issues. Their immune systems might not fight off infection as well. The outcome can be worse too: one study noted that when someone catches Legionnaires’ in a hospital, the death rate can exceed 25%, much higher than the ~10% average for community-acquired cases (Where Does Legionnaires’ Disease Come From? – Legionnaires’ Disease Attorney).
- Examples: There have been numerous hospital outbreaks. For instance, a few years ago in Pittsburgh, a hospital had to notify patients after Legionella was found in its faucet water. In Illinois, a veterans’ home (a long-term care facility) experienced a Legionnaires’ outbreak that took multiple lives. Such cases often make headlines because of the vulnerability of the victims.
Healthcare facilities are expected to follow strict guidelines to prevent Legionella. Organizations like the CDC and Centers for Medicare & Medicaid Services (CMS) urge hospitals to have effective water management programs. This includes routine water testing, maintaining water heaters at proper temperatures, cleaning showerheads, and installing filters where needed.
Senior Living Facilities
Senior living communities and assisted living facilities house populations that are highly susceptible to Legionnaires’ disease. Many residents are elderly or have chronic illnesses, which means even a small exposure to Legionella can cause severe illness.
These facilities often have the same risk factors as hospitals: large plumbing networks, communal showers, decorative water features, and sometimes on-site physical therapy pools or hot tubs.
Prevention is key: Senior facilities should regularly flush their water systems and monitor chlorine levels. Some states even have specific regulations for nursing homes to test for Legionella after any positive case. When those protocols aren’t followed, it’s the residents who pay the price. Families of nursing home residents who suffer or die from Legionnaires’ disease can pursue wrongful death lawsuits against the facility for failing to protect their loved ones.
If your parent or loved one contracted Legionnaires’ at a senior facility, please see our section on Wrongful Death Lawsuits or contact us for compassionate guidance. We understand how devastating this can be.
Office Buildings and Industrial Facilities
Large office buildings, factories, and other commercial buildings often use complex water systems and cooling towers, just like hotels. A cooling tower on an office roof that’s teeming with Legionella can spread bacteria through the air over a wide area, affecting not just the building’s occupants but even people nearby. There have been downtown outbreaks where multiple buildings’ cooling towers were found positive during a public health investigation.
Workplace exposure: If you contracted Legionnaires’ disease and suspect it was from your workplace (for example, you work in a particular building and multiple coworkers also got sick), this might be both a personal injury case and potentially a workers’ compensation case. Our attorneys can advise on the best route, but in general, if a building owner’s negligence caused an outbreak, they can be liable to all affected – employees, visitors, or the public.
Other Uncommon Sources (Water Heaters, Soil, and More)
While most cases come from the sources above, Legionnaires’ disease can from anywhere that gets Legionella bacteria in a person’s lungs:
- Home Water Systems: Though rarer, sometimes a person contracts Legionnaires’ from their own home – for instance, if a home hot-water heater is set too low (<120°F) and the person is at risk (elderly or immunocompromised). If you rent your home, a landlord could be responsible for failing to provide safe water. If you own, it’s more about awareness and prevention.
- Construction Sites and Potting Soil: Certain Legionella species live in soil and compost. Gardeners and construction workers have contracted Legionnaires’ by stirring up contaminated dirt or potting mix and breathing in the dust. In New Zealand and Australia, potting soil is a known source of Legionella infections, prompting warnings on gardening products. In the U.S., it’s less frequent but still possible. If a bag of commercial potting mix was contaminated and caused illness, the manufacturer and seller of the contaminated potting soil may be liable for damages.
- Water Births: A very rare but notable source is water birth pools (tubs used for labor/delivery). They have been linked to infant Legionnaires’ disease cases when the water wasn’t properly treated.
- Medical Equipment: Additionally, things like ventilators or respiratory therapy devices that use tap water can aerosolize Legionella if the water was contaminated. In one instance, Legionella was transmitted through a lung transplant because the donor had aspirated contaminated river water before death.
We Find the Source – and Hold Them Accountable
Determining exactly where Legionella came from in your case is a key step in getting justice. Our legal team works closely with scientific experts and health departments to trace outbreaks to their root. We’ve investigated Legionnaires’ disease cases stemming from hotels, hospitals, senior homes, factories, and more. Once we identify the source, we work to pinpoint who was responsible for maintaining that system.
When an outbreak is confirmed, it’s common for a health department to issue reports or citations against the facility involved. We use those findings – along with our independent investigation – as evidence in your case. Whether it’s a hotel chain, a hospital, a property management company, or a maintenance contractor, if their negligence led to the Legionella exposure that made you or your loved one sick, we will build a strong claim against them.
Bottom line: Legionnaires’ disease comes from unsafe water practices. The good news is that it’s preventable – and when it’s not prevented, victims have the right to seek answers and compensation. We encourage you to reach out to us so we can start investigating. Time is critical, as sources can be cleaned up quickly after people fall ill, potentially destroying evidence – so the sooner we can get involved, the better.
Contact us for a Free Consultation
If you or a loved one contracted Legionnaires’ disease, you need to hire a lawyer with experience handling cases like yours to get the best possible result. An experienced Legionnaires’ lawyer will thoroughly investigate your case to determine the source of your Legionella pneumonia infection and identify the liable parties that can be sued.
Pritzker Hageman is one of the few law firms in the country that has obtained multi-million-dollar recoveries in Legionnaires’ disease lawsuits. With a proven track record of success and over four decades of experience, our legal team knows how to conduct an independent investigation to lay the groundwork for a lawsuit against the facility whose unsafe water caused your illness.
Contact the Pritzker Hageman Legionnaires’ Disease Lawyers
Phone: 1-888-377-8900 | Text: 612-261-0856
Our award-winning Legionnaires’ legal team handles cases for clients in every state in the country.
History of the First Reported Legionnaires’ Disease Outbreak
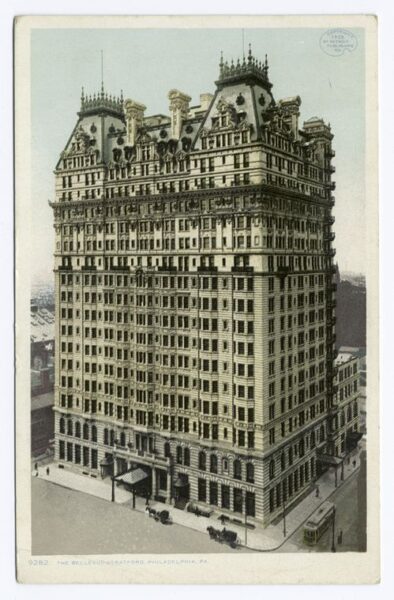
A hotel was the site of the first Legionnaires’ disease outbreak reported in the United States. In 1976, more than 200 people were sickened and 34 died in a Legionella pneumonia outbreak at the Bellevue Stratford Hotel in Philadelphia.
At the time, the hotel was hosting the 58th annual convention for Pennsylvania members of the American Legion, which is where the name “Legionnaires’ disease” comes from.
It took CDC microbiologist Dr. Joseph McDade six months to discover the pathogen that caused the outbreak. Investigators found that the outbreak source was the cooling tower for the hotel’s air conditioning system, which prompted new regulations for climate control systems worldwide.
After the discovery of Legionella, health officials identified Legionnaires’ disease as the cause of past outbreaks. Scientists determined that the first known Legionnaires’ outbreak in the United States happened in 1957 at the Hormel meat-packing plant in Austin, Minnesota.
